For the 2022-2023 grant cycle, the University of Arizona Sarver Heart Center awarded five Investigator Awards.
Opening the black box: The intervention-to-outcome gap in cardiogenic shock complicating acute myocardial infarction
 Scientist: Deepak Acharya, MD, MSPH, associate professor of medicine
Scientist: Deepak Acharya, MD, MSPH, associate professor of medicineCardiogenic shock, a condition where the heart fails to pump blood effectively to vital organs, is a leading cause of death after heart attacks, claiming the lives of nearly half of affected patients. Despite two decades of research, no new treatments have been proven to increase survival of patient in cardiogenic shock. This research aims to unravel the underlying causes of cardiogenic shock and uncover new treatment approaches that can significantly improve patient care and outcomes.
Dr. Acharya’s research will focus on three specific questions. Firstly, to explore how different therapies influence the size of heart tissue damage caused by heart attacks, as reducing this damage could potentially lead to earlier resolution of cardiogenic shock and prevent heart failure. Secondly, he will assess the impact of different therapies on end-organ perfusion, as the clinical outcomes of cardiogenic shock are closely tied to the adequate blood supply to organs such as the brain, kidney, and liver. Finally, the study aims to understand the complex interplay between therapies, infarction size, systemic perfusion, and systemic inflammatory response. It is crucial to define these relationships to ensure that improvements in one aspect do not have unintended negative effects on other factors.
By answering these critical questions, this research project seeks to pave the way for novel treatment approaches that can save lives and enhance the care of patients experiencing cardiogenic shock. The findings will guide clinicians in selecting the most effective therapies based on individual patient needs, ultimately leading to improved outcomes and a brighter future for those affected by this life-threatening condition.
New mechanisms underlying cardiac contractility and failure
Heart failure is the most common outcome of cardiovascular diseases. It is a complex disease, with multiple etiologies and high mortality rates. Dr. Chignalia aims to enhance our understanding of the early molecular mechanisms underlying heart failure, specifically focusing on the role of a macromolecule called glypican 1.
The research team hypothesizes that glypican 1, found on the surface of heart muscle cells, plays a vital role in regulating cardiac function and contractility. By investigating the influence of glypican 1, they aim to identify key factors involved in heart function and calcium levels, which are critical for determining the strength of each heartbeat. Understanding the impact of glypican 1 on heart development and function could lead to the identification of new targets for drug development to treat heart failure.
To explore this hypothesis, Dr. Chignalia and the team will utilize innovative techniques and approaches. They will study the effects of glypican 1 deficiency on heart contractility using advanced in vivo and ex vivo methods. Echocardiography will be used to measure cardiac output and assess heart function indirectly. Additionally, isolated heart strip preparations will allow for direct measurement of contractile force.
Pharmacological inhibitors will be used to determine the specific calcium channels regulated by glypican 1. Furthermore, the researchers will investigate if altered calcium storage within the cells contributes to heart failure. The findings from this study will expand our knowledge of the role of glypican 1 in heart function and provide insights into potential therapeutic targets for treating heart failure.
By advancing our understanding of the molecular mechanisms underlying heart failure, this research has the potential to pave the way for the development of innovative treatments that improve patient survival and reduce the burden of heart failure on healthcare systems. The data generated from this study will lay the foundation for future research endeavors, further enhancing our understanding of heart failure and guiding future drug development efforts.
Orange fluorescent protein cardiac myosin-binding protein C biosensor
 Scientists: Brett Colson, PhD, associate professor
Scientists: Brett Colson, PhD, associate professorDr. Colson aims to revolutionize the screening process for new drugs targeting life-threatening diseases like heart failure. By leveraging advanced fluorescence instrumentation, researchers seek to explore the fundamental question of how myosin-binding protein C (MyBPC) interacts with actin and myosin under various physiological conditions in the heart. The pilot data obtained will support a future NIH R01 proposal for mechanistic and therapeutic investigations led by Dr. Colson.
Previous funding enabled the successful development of a genetically-encoded Orange Fluorescent Protein (OFP)-biosensor tag on MyBPC, confirming specific expression of the tagged protein. Initial assessments show normal heart structure and absence of abnormalities. However, further validation is necessary through comprehensive studies such as echocardiography, pressure-volume loop analysis, and histology to ensure normal heart function.
To confirm the suitability of the proposed model for mechanistic studies, the team plans to conduct Fluorescence Resonance Energy Transfer (FRET) experiments using genetically-modified muscle fibers. By introducing an acceptor molecule, they aim to measure distances and investigate the interactions between MyBPC, actin, and myosin. Successful outcomes will lay the groundwork for high-throughput drug screening, where the model can be utilized to identify small molecules influencing MyBPC's binding to actin or myosin. Such drugs hold promise for enhancing cardiac contractility and potentially treating heart failure and cardiomyopathy.
This innovative research project combines cutting-edge fluorescence techniques and drug discovery efforts to deepen our understanding of heart function and identify potential therapeutic interventions. By advancing our knowledge of molecular interactions and enabling the discovery of novel drugs, this study has the potential to transform the treatment of life-threatening cardiovascular conditions.
Gene and protein expression in an atrial fibrillation model
Atrial fibrillation (AFib) affects millions of people and contributes to thousands of deaths annually. Current treatment options have high recurrence rates and potential side effects. Understanding the genetic changes underlying AFib could lead to more effective therapies. Dr. Moukabary aims to investigate genetic expression patterns in AFib using next-generation RNA sequencing. Unlike previous studies focusing on specific areas of the heart, this research will comprehensively examine gene expression throughout the left atrium, right atrium, and left atrial appendage.
Collaborating with fellow Sarver Heart Center members Jared Churko, PhD, and Steve Goldman, MD, the research team will provide valuable insights into the molecular mechanisms of AFib, shedding light on the genes and proteins involved in the disease. Additionally, the team plans to utilize specialized human heart cells generated in the laboratory to gain further insights into gene activation and explore novel treatment approaches. This study could pave the way for advancements in the treatment of AFib and potentially lead to personalized treatment approaches based on genetic profiles.
Ultimately, this research aims to define the genes affected by persistent AFib and explore regulatory elements and pathways that could be targeted for gene regulation, opening new possibilities for effective AFib treatments.
Redesigning chart review for the modern era through problem-centric data visualization
 Scientists: Jeffrey Tran, MD, cardiovascular disease fellow, Nancy Sweitzer, MD, PhD, and Olivia Hung, MD
Scientists: Jeffrey Tran, MD, cardiovascular disease fellow, Nancy Sweitzer, MD, PhD, and Olivia Hung, MDNavigating electronic health records (EHRs) poses significant challenges for healthcare providers, leading to medical errors and frustration. Dr. Tran aims to address these issues by redesigning the EHR interface and improving the chart review process, starting with chronic cardiovascular disease management.
The current EHR interface mimics paper charts, making it difficult for clinicians to assemble relevant patient data from various sources. This process, called chart review, is time-consuming, cognitively demanding, and error-prone. With the rising complexity of healthcare data and limited review time, incomplete data analysis becomes a risk, potentially compromising patient safety.
To overcome these challenges, the research team plans to develop a problem-centric data visualization application that presents all relevant patient information in a single display. This approach aims to simplify data aggregation, reduce cognitive load, and enhance the accuracy and efficiency of medical decision-making. The application will focus on chronic cardiovascular diseases, leveraging the expertise of cardiologists and professional medical society guidelines.
The team will collaborate with experienced Silicon Valley developers to build and refine the application, incorporating iterative feedback from cardiovascular experts. Through this project, they seek to gain a deeper understanding of chart review challenges and demonstrate the potential of the problem-centric data visualization solution to improve workflow and patient care. The preliminary evidence generated will support future grant applications for further development and comprehensive investigation.
By improving the usability of EHRs and streamlining the chart review process, this research aims to reduce medical errors, enhance clinical decision-making, and ultimately improve patient outcomes. The proposed solution has the potential to transform healthcare by facilitating rapid access to comprehensive patient data, reducing cognitive overload, and enabling more accurate diagnosis and treatment of chronic cardiovascular diseases.


 Scientists:
Scientists: 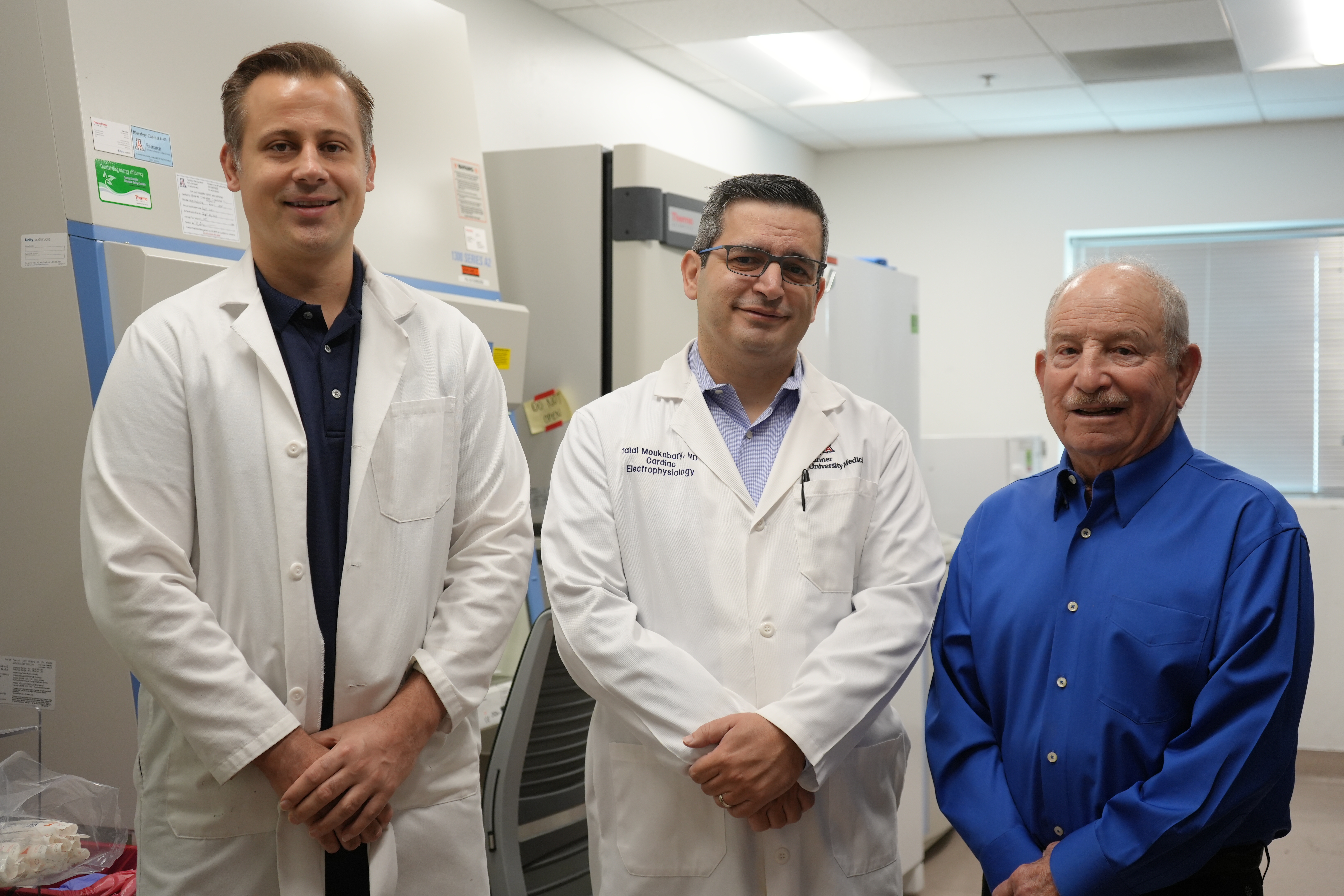 Scientists:
Scientists: