An observational clinical study launched at Sarver Heart Center seeks to improve patient treatment and satisfaction with preventive cardiovascular disease (CVD) care.
“We hope this information will help the physicians provide the most appropriate and aggressive preventive CVD care, minimize the rate of adverse drug effects, and increase patient engagement and satisfaction with treatment. We also hope to receive feedback from our participating clinicians in order to give us insight on the how best to provide doctors with useful, actionable information,” said Joseph Alpert, MD, professor of medicine who is leading this study.
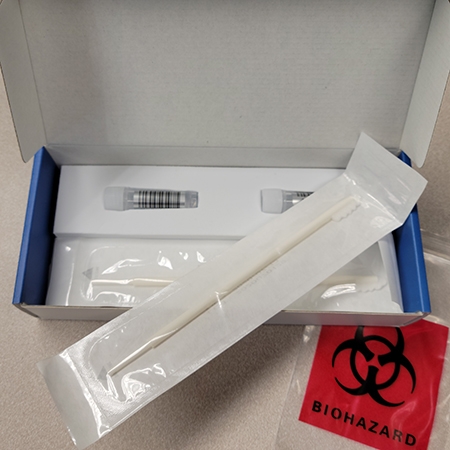
Genetic screening for a broad range of CVD-related variants is performed including:
- Familial Hypercholesterolemia (FH), a genetic condition in which the body is unable to remove low density lipoprotein (LDL) cholesterol from the blood, resulting in elevated levels of LDL, or “bad” cholesterol.
- Factor V Leiden Thrombophilia, an abnormality in blood clotting that increases the chance of blood clot formation within blood vessels and may contribute to CVD.
- Hyperthyroidism, an active thyroid hormone affects blood vessel elasticity, which may cause blood pressure changes to compensate for increased vascular resistance, increasing the chance of CVD. Levels of active thyroid hormone also influence cholesterol levels.
- Type II Diabetes, compared to those without diabetes, adult diabetics are between two and four times more likely to die from CVD.
The study also will assess variants in drug metabolism and drug transport genes that may affect CVD treatment. Drug response can vary between people due to genetic composition. Genetic screening of drug metabolism and transport genes (CYP2C19, CYP2D6, CYP2C9, VKORC1, and SLCO1B1), may help physicians better gauge the risk of adverse drug effects or need for alternate dosing strategies. This patient-specific information may also lead to increased patient satisfaction and engagement with preventive treatment, making the patient more likely to adhere to their prescribed treatment.
This is one example of the more than 20 clinical research studies underway in Sarver Heart Center’s Cardiovascular Clinical Research Program. To learn more about clinical research at Sarver Heart Center, visit SARVER HEART CENTER CLINICAL RESEARCH

