By Elizabeth Juneman, MD
Associate Professor of Medicine, Division of Cardiology at the University of Arizona College of Medicine - Tucson
University of Arizona Sarver Heart Center
When it comes to women’s health, should we be looking more deeply into matters of a women’s chest, not just the breast? For millennia, women’s breasts have been the focus of cultural attention. When you consider today’s medical and social focus on breast cancer prevention, you have to wonder whether this creates tunnel vision when it comes to women’s health.
While breast cancer is an important concern, are we misdirecting our point of focus? After all, heart disease is the leading cause of death in women.
Consider the statistics: 1 in 3 women will die from cardiovascular disease, compared with 1 in 31 who will die from breast cancer. Heart disease doesn’t discriminate; it is the leading cause of death whether you’re black, white or Latina.
If you think this is your grandmother’s health concern, bear in mind that heart disease occurs in 1 in 9 women ages 45 to 65. At every age from 45 up, more women die from heart disease than from cancer.
Are you ready to go beyond the “bikini” view of women’s health; beyond the focus on the breasts and reproductive organs?
Know and Manage Your Risks
Start young. Guidelines recommend that you start screening for heart disease risk at age 20.
Screening When to have it
Weight and body mass index (BMI) Each healthcare visit beginning at age 20
Waist circumference Each healthcare visit if BMI is 25 or more
Blood pressure Each visit or at least once every two years
Cholesterol levels Every four to six years for normal-risk people; more for those with elevated risk factors for heart disease
Glucose levels At pregnancy or at least every three years after age 45
Smoking, physical activity and nutrition Each healthcare visit
Did you know?
Three of every 4 women with high blood pressure know they have it. Fewer than 1 in 3 are controlling it.
Women also have modifiable risk factors related to estrogen status and inflammatory markers. By the time women reach age 65, 20 percent have two or more risk factors and 40 percent have multiple risk factors.
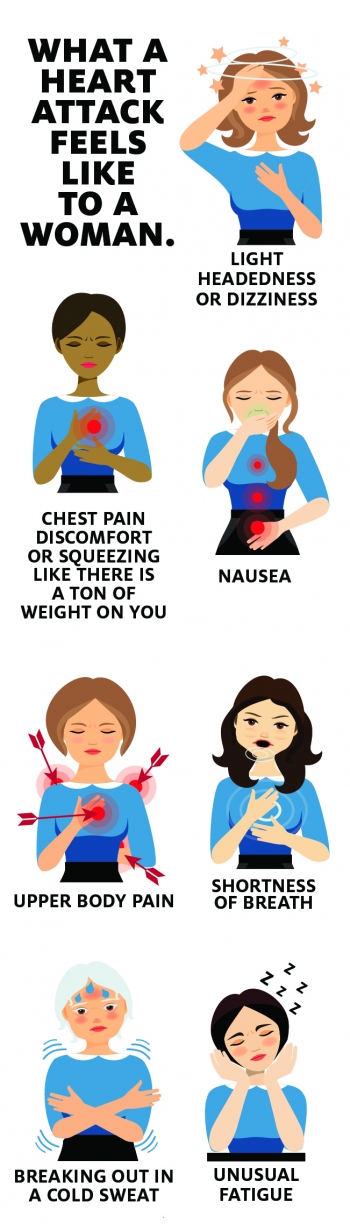
Know Heart Attack Symptoms – The Usual and Unusual
Women are different than men. Usual heart attack symptoms include discomfort or pressure type feeling behind the breast bone. This may be a burning, heavy or squeezing feeling. This discomfort may intensify with exertion, stress or emotions, and be relieved by rest or nitroglycerin pills.
Some women don’t experience the usual “textbook” chest pressure during a heart attack. Women are more likely to have unusual symptoms, including:
- Pain in the back, abdomen, jaw or arm, which may be sharp or fleeting, or repeated or very prolonged
- Shortness of breath
- Nausea or vomiting
- Unrelated to exercise
- Not relieved with nitro pills or rest
- Relieved with antacids
- Palpitations without chest pain
Here are some other ways women and men are different:
- Since 1984, the number of heart disease deaths for females has exceeded those for males.
- While heart disease typically strikes at an older age in women compared to men, women are more likely to also have untreated high blood pressure, obesity, diabetes, high cholesterol, more persistent symptoms and require more hospitalizations for chest discomfort.
- Women who suffer a sudden cardiac arrest are more likely to die prior to arriving at the hospital, to die in the year following a heart attack, to have a second heart attack, and to have heart failure.
- Women are less likely to have large blocked arteries, but can have disease in the smaller arteries. Women with heart disease have a higher mortality compared with similarly aged men.
- Women also are more likely to have microvascular dysfunction, called Cardiac Syndrome X, which causes chest pain with decreased blood flow to heart tissue but normal coronary arteries.
- Women are more likely to have stress cardiomyopathy, also called “Takotsubo” or “Broken Heart” syndrome – heart muscle weakness caused by intense mental stress, emotional pain or trauma.
- Women are less likely to be evaluated for heart disease, undergo stress testing, cardiac catheterization and receive medication for control of risk factors.
Be Your Best Advocate
Make sure your doctor doesn’t have a “bikini” view of women’s health. Discuss your risks for heart disease and ask your doctor about the biological differences between men and women when it comes to heart disease symptoms, tests and complications.
We 'Go Red for Women' the first Friday in February and focus on women and heart disease always.


