09/04/14
Original Story Link: http://opa.uahs.arizona.edu/newsroom/news/2014/three-most-important-ques...
 Atrial fibrillation, the most common heart-rhythm abnormality, affects 2 to 3 million people in the United States, a number projected to increase to 12 million by 2050 as the population ages, according to the U.S. Centers for Disease Control and Prevention. September is National Atrial Fibrillation Awareness Month and a good time to talk to your doctor about this condition that increases your stroke risk.
Atrial fibrillation, the most common heart-rhythm abnormality, affects 2 to 3 million people in the United States, a number projected to increase to 12 million by 2050 as the population ages, according to the U.S. Centers for Disease Control and Prevention. September is National Atrial Fibrillation Awareness Month and a good time to talk to your doctor about this condition that increases your stroke risk.
Here are three recommended atrial fibrillation (a-fib) questions from Julia H. Indik, MD, PhD, professor of medicine at the University of Arizona Sarver Heart Center and a cardiologist who specializes in evaluating and treating heart-rhythm disturbances.
 1. What is my risk for stroke?
1. What is my risk for stroke?
Learn your CHADS-VASc score. This is a stroke risk calculation for patients with a-fib, said Dr. Indik. Points are added if you have heart failure, high blood pressure, diabetes, history of stroke (even a “mini-stroke”) or vascular disease, are 65 to 74 years old (add an extra point at 75 years or older), or are a woman. If you have a-fib, your doctor will use this score to recommend appropriate blood thinning therapy, with a goal of preventing blood clots that can cause a stroke. If your score is 0, your risk of stroke is extremely low and you probably don’t need any blood thinners. However, if your score is 2 or higher, you’ll likely get a prescription for warfarin or another blood thinner. If your score is 1, you and your doctor need to weigh the risks and benefits together.
2. Is it better for me to control my heart rhythm or my heart rate?
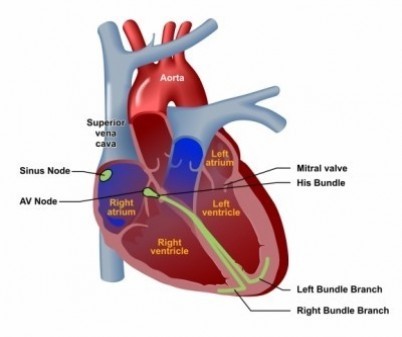
“This depends on your symptoms and health history,” said Dr. Indik. Common a-fib symptoms are breathlessness, lack of endurance, a racing, irregular or uncomfortable heart rate, and a minority of patients may develop heart failure. Medication management, using the same drugs prescribed for controlling high blood pressure, is the low-risk way to control heart rate. For many patients, if heart rate is controlled and symptoms minimized, this is the best management strategy. Older and more frail patients sometimes don’t tolerate the rate-control medications. In such cases, doctors may recommend implanting a pacemaker together with a procedure to create a block in the heart rhythm’s path. This will control the heart rate without medications, but does require an invasive procedure. In select patients, restoring the heart rhythm to normal may be preferable to heart-rate control. To restore a normal rhythm, your doctor may prescribe medications or order a rhythm-restoring procedure called ablation of the left atrium. In this procedure, which is performed in the electrophysiology laboratory, areas of the left atrium (the upper chamber of the left side of the heart) known to be involved in generating the atrial fibrillation are cauterized (or burned) to reduce the chances that atrial fibrillation can start up or continue.
3. What can I do to prevent atrial fibrillation?
If you smoke, quit. If you have high blood pressure, make sure you work with your doctor to bring it down into the recommended range. If you have sleep apnea (snoring, daytime sleepiness) or think you might, get tested and treated. If you’re obese begin, a diet and exercise program that helps promote weight loss. Drink alcohol moderately, if at all. We are all aging, and that is one risk factor you can’t prevent.
For more heart health information, please visit the University of Arizona Sarver Heart Center website. Follow us on [Facebook]*linked to unavailable page* and Twitter @SarverHeart.
Dr. Julia Indik serves on committees of the American College of Cardiology, the American Heart Association and the Heart Rhythm Society, including development of professional education activities and clinical consensus statements and guidelines.
Media Contact: Katie Maass

